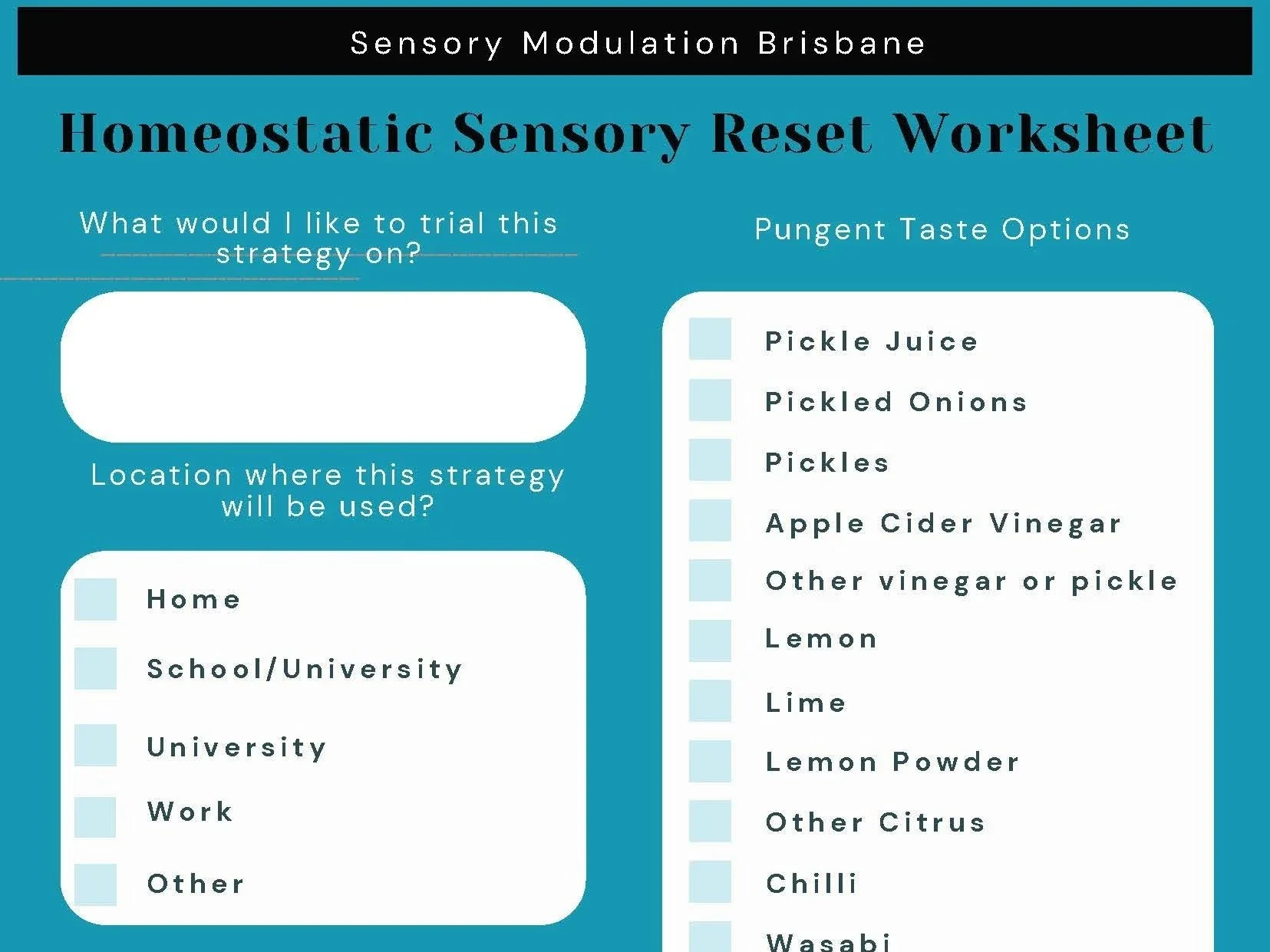
Sensory Modulation Brisbane has developed a worksheet (including a fillable option) to support structured application of the Homeostatic Sensory Reset Hypothesis. The worksheet includes practical considerations to guide safe selection and use of gustatory input within everyday contexts.
Read moreusing Sensory Modulation as an Intervention: DIN
The model proposes that sensory modulation works by addressing the following three constructs:
1. Strengthening sensory awareness for the Person
2. Changing the Environment
3. Changing the Occupation
For each of these three areas, sensory input can be changed by using the acronym DIN -
· Decreasing the sensory input
· Increasing the sensory input
· (introducing) New sensory input
Read moreThe Role of Bubble Columns in Sensory Rooms for Adults: Are They Childlike or Therapeutic?
Sensory rooms are used as spaced for calming and reducing distress in mental health units, schools, nursing homes, shopping centres, sports venues and other community spaces. These rooms are designed to support sensory modulation through calming sensory input such as lighting, textures, sounds, and visual input. One common feature of these rooms, however, raises an important question: the use of bubble columns. These visually appealing, colourful, water-filled tubes are often seen in sensory rooms, but are they still serving their intended purpose, or are they unintentionally reinforcing a sense of infantilisation for adults?
Read moreHot Spots and Hot What’s in Sensory Modulation Interventions
Mental Health Units, Emergency Departments and other hospital and care environments are places where higher levels of aggression and frustration can occur. Within these environments there can be specific locations/areas which have an even greater concentration of aggression and frustration. These locations can be described as Hot Spots. (Gillespie et al 2018). In the safe wards literature, the physical environment is one of six domains or categories of factors that can give rise to flashpoints, which have the capacity to trigger conflict and/or containment. (Bowers, 2014).
This article will explore how to identify Hot Spots (and Hot What’s) and some solutions to address them.
Read moreBlogs Index
Misophonia – more than just dislike of sounds and how OTs can help
Most people can relate to the experience of certain noises or sensations as being really unpleasant. For example, the thought of nails scratching down a blackboard can make the hairs on your arms to stand up, your teeth feel ‘on edge’ and the strong impulse to quickly cover your ears to stop the noise!
The term “misophonia” (hatred of sound) was first used in the early 2000’s to characterise the experience of an extreme emotional and physical response to certain ordinary, often repetitive, day to day sensory input. It is reported to occur in up to 20% of the population and equally in men and women. The input that evokes the most intense responses tends to be human created orofacial noises like breathing, swallowing, chewing, sniffing, throat clearing and lip smacking. Noises such as tapping and pen clicking have also been reported to be problematic. For people with misophonia, these experiences can evoke intense responses that may not seem in keeping with the circumstance such as disgust, irritation, anxiety, distress, anger and an overwhelming desire to remove themselves or remove the input from their environment.
Rather than misophonia being a hearing problem, it is now proposed to stem from attentional or emotional processing issues later in the brain’s auditory system. In examining brain activity while listening to a variety of sounds (including neutral, unpleasant and known misophonia triggers) Kumar et al (2017) found the following:
· the misophonia group rated the trigger sounds as more distressing than the other sounds.
· the research control group rated trigger and unpleasant sounds as similarly annoying.
Read morePredictive processing, sensory processing and motor control
Woman with long hair and white dress walking down some steps that look wobbly.
This blog is part of a series on the implications of predictive processing for clinical practice.
Several people have asked us about praxis and predictive processing and we thought it was useful to write a separate blog on this. We will start by discussing 2 models of sensory processing.
1. Classic detector model of sensory processing. This has been the model for years.
2. Predictive processing model of sensory processing. This is now the leading model of sensory processing in neuroscience literature but is less well known in the clinical area.
Read moreMultisensory top down templates and multi sensory integration
2023 has had a number of articles released on multi sensory integration with some important findings including:
· Multisensory functional brain networks
· Multisensory templates as a top down process
· Multisensory processing occurring at earliest stages of information processing.
Some of the important points from these articles have been included but they are worth reading in their entirety if you are interested in this area.
Read more
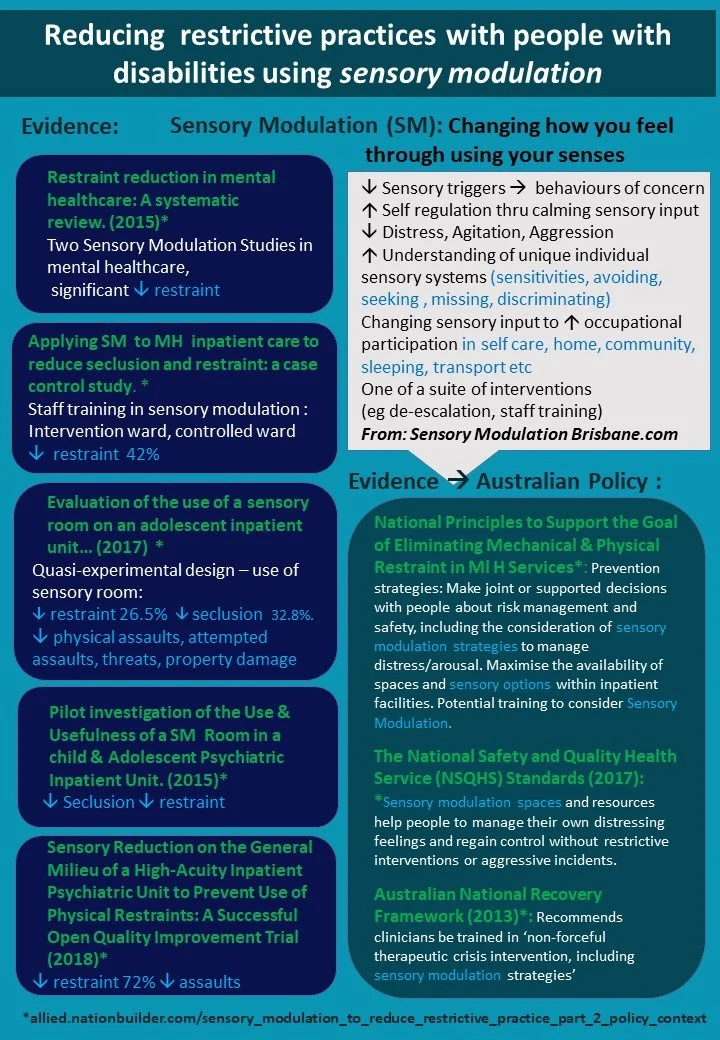
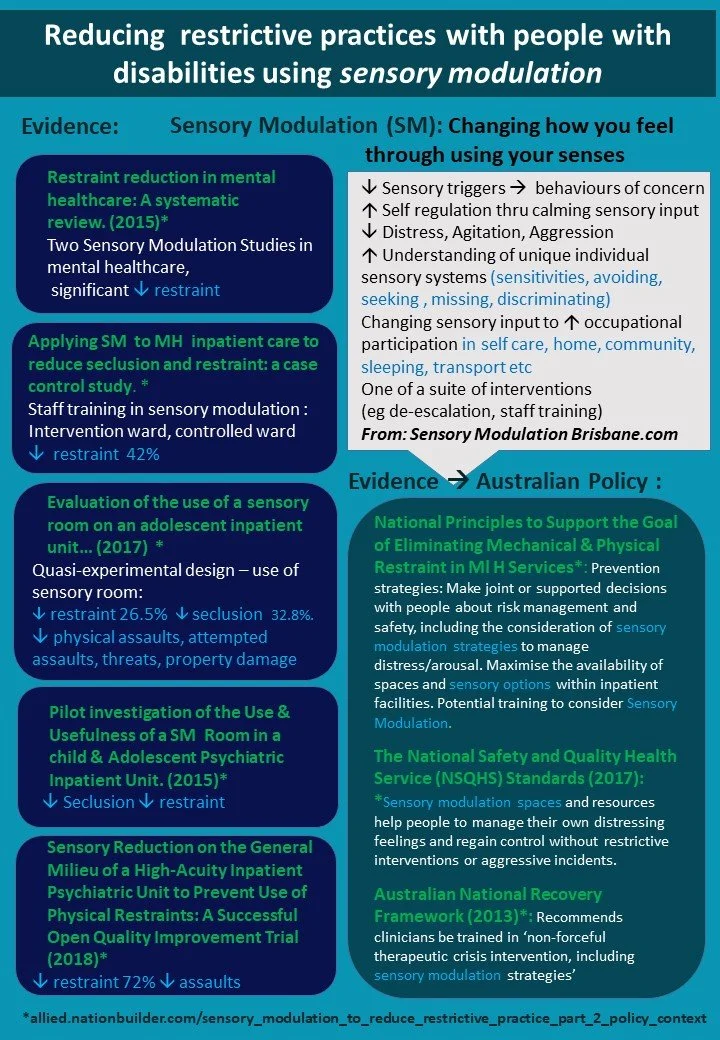
Evidence base for sensory modulation in the reduction of restrictive practice for NDIS participants
Evidence base for Sensory Modulation in the reduction of restrictive practices for NDIS participants
We have recorded a presentation and this is available on youtube.
The reference list for this presentation is available here:
Read morePredictive Processing and Body image disturbance in Anorexia Nervosa
When a person with Anorexia Nervosa looks in the mirror, they often report seeing someone who is very overweight rather than the thin body that they actually have.
In the classic detector model of sensory processing, it can be hard to understand how the person can see something that is not reality.
Predictive processing* provides another explanation. that the person is seeing the brains prior model or prediction that they will see, and due to the stress of the condition , they are ‘stuck’ on the predicted model unable to see the reality. A persons predictions are built up from prior experiences and also information from interoception ie feeling fat.
Read morePredictive processing: a leading theoretical framework for sensory processing
Predictive Processing is a computational theory of brain functioning where the brain continuously works to minimise error between existing model-based predictions and incoming information (May et al 2021). The theory asserts that the brain generates prior models or predictions of sensory input at multiple levels, generating expectations or inferences regarding future input. This function serves to minimise uncertainties and maximise efficiencies (Wilkinson et al, 2017). Predictive processing as a theory also helps to explain the large number of descending connections in the brain (Walsh et al 2020). In the instances where unpredicted or unexpected sensory input is detected (referred to as a prediction error) this information may pass through these multiple layer and then can update the prior model.
Predictive Processing has been described as “A leading theoretical framework for Sensory Processing” (Tabas et al 2021) and has a lot of ‘explanatory power’ for mental health and sensory processing clinical areas.
When we consider that the brain is largely predicting rather than reacting to sensory input, it may have clinical implications for OTs.
Read moreSniff research in Autism
Scent research in Autism
An older article from 2015 on scent and sniffing pleasant and unpleasant odors, noted that Autistics sniffed at pleasant and unpleasant odors with the same intensity whereas neurotypicals sniffed more intensely with pleasant odors and less intensely with unpleasant odors.
We wonder if the more intense sniff is increasing the intensity of the scent and thus contributing to increased sensory overwhelm to scent?
We would love to see some research into whether this could be developed into an easy intervention. We searched articles this week and could not find interventions but please let us know if there are some.
We would propose an intervention where Autistic children could learn to visually identify potentially unpleasant scents (this would need to be individually tailored) and also learn to control the intensity of their sniff to decrease the overwhelm. This could focus on scents that are more commonplace in everyday environments (schools, shops) and where the scent is impacting on occupations.
It has been difficult to research the olfactory (scent) sense in Autism, partly due to the difficulties with accuracy of measurement. A new precise and easy to use system has been developed – the odor pulse ejection system. It is described in this article:
https://www.frontiersin.org/articles/10.3389/fnhum.2020.523456/full
This system was designed to more accurately measure olfactory processing including odor detection, identification and evaluation. Findings of the study using the odor pulse ejection system suggest differences in aspects of olfactory processing for autistics, including olfactory working memory and/or attention.
Xu, M., Minagawa, Y., Kumazaki, H., Okada, K., & Naoi, N. (2020). Prefrontal Responses to Odors in Individuals With Autism Spectrum Disorders: Functional NIRS Measurement Combined With a Fragrance Pulse Ejection System. Frontiers in Human Neuroscience, 14. https://doi.org/10.3389/fnhum.2020.523456
Read moreProviding choice of menstrual products in Mental Health Unit Design
Sensory sensitivities are common in people with mental illness and Autistics and (1)
can impact on periods & menstrual products. This can include:
· touch
· visual input
· scent
· coordination and fine motor skills
· trauma
· pain and Interoception
· familiarity and uncertainty
Touch
When choosing menstrual products, there can be a variety of different preferences for touch sensations in menstrual products This includes the feeling of a tampon and cup (sometimes lubricant changes the dry tampon feeling) or the feeling of a bulky pad in underwear, or the feeling of the pad against the skin. If new to menstrual cycles it is useful to explore what option is the most comfortable. If the person has a preference then it is important to enable access to this preference. . When someone is sensitive to touch they can be unable to get used to (habituate) a sensation and this can be very irritating, distressing or overwhelming.
Read moreSensory Assault
This blog is a commentary on a recent article by Beth Ohannesson Sarah Schoen, Vanessa Mitchell B Parent perspectives on children with sensory over-responsivity. The article describes a study in which parents of children with sensory over responsivity and sensory meltdowns/ sensory over responsivity episodes described their childrens description of the episodes and the strategies that they used to manage them.
Read moreBlogs Index
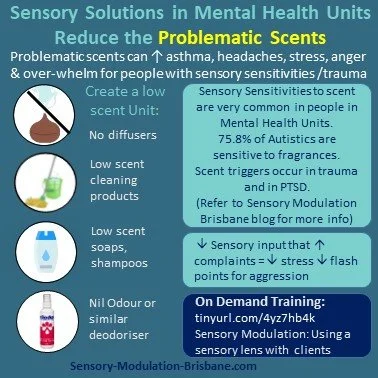
Low scent, fragrances in Mental Health Unit Design
The prevalence of fragrance sensitivities were investigated in the United States, United kingdom, Australia and Sweden by Steinemann (2019) and results included:
· 75.8% of Autistics are sensitive to fragrances
· 26% of the general population report being diagnosed with asthma/asthma like conditions and 57.8% are also fragrance sensitive.
Scents that were particularly problematic included:
· Air fresheners and deodorisers (54.8%)
· Being in a room with recently cleaned products (53.8%)
· Being near someone wearing a fragranced product (56.5%)
Read moreTherapy rooms and waiting rooms: designing for sensory needs
Therapy room with grey lounge, green cushions, a white blanket and a plant on a small table. We would remove the aromatherapy sticks though!
At Sensory Modulation Brisbane, we have been advocating for Universal Design in Mental Health Units for Sensory Sensitivities and we would recommend that this is expanded to therapy rooms, waiting rooms and all health care spaces.
Many people who attend Therapy practices have sensory processing patterns that are more sensitive, more avoiding, or more seeking or more missing of sensations than others and this can vary between different senses. This includes:
· Autistics have sensory processing differences recognised as a diagnostic criteria. (DSM5)
· People with PTSD often have reactivity and hypervigilance to certain sensations
· People with schizophrenia often have auditory processing and visual perception challenges.
· ADHDers frequently have sensory processing differences (Schulze 2020)
· A high percentage of people with mental illness have interoceptive difficulties
Read moreSensory Kits , Trauma Informed Practice and NDIS
Using Sensory items to calm and ground are recognized evidence based strategies.
Yet some people in the NDIS scheme are having NDIS Plan Managers refuse to fund sensory items
This blog provides a rationale for the NDIS to make changes to their website and price guide based on two guidelines.
1. The Disability Guidelines for Trauma –Informed Practice: Supporting people with disability who have experienced complex trauma
2. NDIS Quality and Safeguards Commission (2020) Regulated Restrictive Practices Guide
Read moreUsing alternatives to torch light monitoring in Mental Health Unit Design
This blog will outline some of the challenges involved in using torch light to observe clients in mental health units at night and also provide some alternative options. Part of routine mental health care on mental health units is regular observations of people while they are sleeping/lying in bed. These routine observations are undertaken due to their perceived benefit in ensuring safety and wellbeing and to reduce the risk of suicide or severe harm. Nursing staff may need to complete observations up to 4 times per hour overnight and torch light is frequently used.
Read moreAuditory Processing Needs in Mental Health Unit Design
This blog will outline the auditory sensitivities and sensory processing challenges of people admitted to Mental Health Units and offer recommendations with respect to the design of these environments.
People admitted to Mental Health inpatient Units present with a wide range of mental health disorders including schizophrenia, Borderline Personality Disorder, Post Traumatic Stress Disorder and Autism Spectrum Disorder. It is now understood that people with these diagnoses experience a higher rate of sensory sensitivities and other sensory processing challenges compared to the general population (Stromberg et al).
The sensory system we will focus on today is the Auditory system.
Auditory Processing difficulties have been recognised and explored across a range of research areas including:
Occupational Therapy research of sensory processing difficulties (eg Harrison et al)
Lived experience research such as Autistics, people with schizophrenia (eg Stromberg et al)
Neuroscience research of Auditory State Response gating (eg Sugiyama et al )
Diagnostic Criteria such as hypervigilance to sounds in PTSD and sensory over-responsivity in Autism Spectrum Disorder.
Read more